|
|
 |
 |
Dr. Ashay H. Nandeshwar
M. D., (Ayu)(Mumbai)
(Podar Govt. Medical College)
P.G.D.M.L.T., L.Lb. (Sch)
Lecturer V.P.A.M.C.
Sangli |
| Read More |
|
|
|
|
 |
|
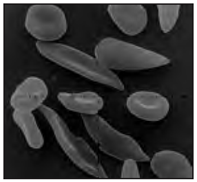
The resulting polypeptide is different and the haemoglobin formed is commonly known as HbS; the normal’ haemoglobin is known as HbA. The result of this is a slightly different structure, by one amino acid of the
haemoglobin molecule which makes it crystallise at low oxygen levels (e.g. in the capillaries). The erythrocyte in which the haemoglobin can be found will then change from a biconcave shape into a sickle-cell shape (see Figure 404) and can block the small capillaries, and is less efficient at transporting oxygen. Even when the oxygen concentration increases again, the cells keep their sickle shape. The symptoms of sickle-cell anaemia are acute anaemia, which causes physical weakness. The lack of oxygen may be severe enough to cause damage to the heart and kidneys or even death (in homozygous individuals). The gene for sickle-cell anaemia is co-dominant with the “normal” allele although the latter is expressed more strongly in the heterozygous individual. Heterozygous individuals (carriers) have some HbS but more normal haemoglobin. They may suffer from mild anaemia. The selective advantage of being a carrier is found in malaria infested areas. Plasmodium (the protist causing malaria) cannot reproduce in erythrocytes with HbS. This means that individuals heterozygous for the sickle-cell trait have a reduced chance of contracting malaria. Natural selection has ensured that the sickle-cell trait is more common among people living in malaria-infested areas such as West Africa. As the African-American population largely originates from this area, the trait is found in frequencies higher than usual in this group. Carriers may not be aware of the fact that they possess the sickle-cell allele and are capable of passing it on to their children. If two carriers have a child, there is a 1 in 4 (25%) chance of the child having the disease.
|
 |
Therefore, it is important that people who may be carriers, are tested to confirm the presence or absence of the sickle cell allele. If a female carrier is pregnant and the father is also a carrier, it is possible to test using amniocentesis or chorionic villi sampling (refer to Topic 4.2.6) to see if the child will have sickle-cell anemia. Should this be the case, then the parents may decide to discontinue the pregnancy. There are no easy answers to this problem. A great deal of research is being done about treating sickle-cell anemia including bone marrow transplant and/or blood stem cell treatment. Gene therapy is also a possibility but research is in an early stage. |
|
| Symptoms: |
Signs and symptoms of sickle cell anaemia usually show up after an infant is 4 months old and may include:
1. Anaemia:
Sickle cells are fragile. They break apart easily and die, leaving you chronically short on red blood cells. Red blood cells usually live for about 120 days before they die and need to be replaced. However, sickle cells die after only 10 to 20 days. The result is a chronic shortage of red blood cells, known as anaemia. Without enough red blood cells in circulation, your body can't get the oxygen it needs to feel energized. That's why anaemia causes fatigue.
2. Episodes of pain:
Periodic episodes of pain, called crises, are a major symptom of sickle cell anaemia. Pain develops when sickle-shaped red blood cells block blood flow through tiny blood vessels to your chest, abdomen and joints. Pain can also occur in your bones. The pain may vary in intensity and can last for a few hours to a few weeks. Some people experience only a few episodes of pain. Others experience a dozen or more crises a year. If a crisis is severe enough, you may need hospitalization so that pain medication can be injected into your veins (intravenously).
3. Hand-foot syndrome:
Swollen hands and feet may be the first signs of sickle cell anaemia in babies. The swelling is caused by sickle-shaped red blood cells blocking blood flow out of their hands and feet.
4. Jaundice:
Jaundice is a yellowing of the skin and eyes that occurs because of liver damage or dysfunction. Occasionally, people who have sickle cell anaemia have some degree of jaundice because the liver, which filters harmful substances from the blood, is overwhelmed by the rapid breakdown of red blood cells. In people with dark skin, jaundice is visible mostly as yellowing of the whites of the eyes.
5. Frequent infections:
Sickle cells can damage your spleen, an organ that fights infection. This may make you more vulnerable to infections. Doctors commonly give infants and children with sickle cell anaemia antibiotics to prevent potentially life-threatening infections, such as pneumonia.
6. Delayed growth:
Red blood cells provide your body with the oxygen and nutrients you need for growth. A shortage of healthy red blood cells can slow growth in infants and children and delay puberty in teenagers.
7. Vision problems:
Some people with sickle cell anaemia experience vision problems. Tiny blood vessels that supply your eyes may become plugged with sickle cells. This can damage the retina — the portion of the eye that processes visual images. |
| |
|
|
|